Hauptfolge März 2025 – Folge 75
Der Frühling naht und auch im März erwartet euch ein brandneuer Journalclub. Außerdem wird es diesen Monat mal wieder nerdig: Wenn ihr was darüber lernen möchtet, was ihr als Intensiv- und Notfallmediziner:innen über die neue „Wunderwaffe“ der Onkologie wissen solltet und über Anästhesie bei Rothaarigen, dann hört rein!
Journal Club:
Paula:
Jian, SJ.Z., Cheng, TH. & Yen, CC. Prognostic accuracy of point-of-care ultrasound in patients with pulseless electrical activity: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 33, 27 (2025). https://doi.org/10.1186/s13049-025-01327-0
George TS, Ashburn NP, Snavely AC, Beaver BP, Chado MA, Cannon H, Costa CG, Winslow JE, Nelson RD, Stopyra JP, Mahler SA. Does Single Dose Epinephrine Improve Outcomes for Patients with Out-of-Hospital Cardiac Arrest and Bystander CPR or a Shockable Rhythm? Prehosp Emerg Care. 2025;29(1):37-45. doi: 10.1080/10903127.2024.2348663. Epub 2024 May 21. PMID: 38713769; PMCID: PMC11579245.
Thorben:
Dominic:
Flynn SG, Park RS, Jena AB, Staffa SJ, Kim SY, Clarke JD, Pham IV, Lukovits KE, Huang SX, Sideridis GD, Bernier RS, Fiadjoe JE, Weinstock PH, Peyton JM, Stein ML, Kovatsis PG. Coaching inexperienced clinicians before a high stakes medical procedure: randomized clinical trial. BMJ. 2024 Dec 16;387:e080924. doi: 10.1136/bmj-2024-080924. PMID: 39681397; PMCID: PMC11648086
Anästhesie bei Rothaarigen
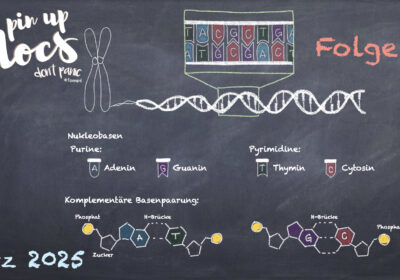
Grundlagen Biochemie / Physiologie
Schaffer JV, Bolognia JL. The melanocortin-1 receptor: red hair and beyond. Arch Dermatol. 2001 Nov;137(11):1477-85. doi: 10.1001/archderm.137.11.1477. PMID: 11708951.
Xia Y, Wikberg JE, Chhajlani V. Expression of melanocortin 1 receptor in periaqueductal gray matter. Neuroreport. 1995 Nov 13;6(16):2193-6. doi: 10.1097/00001756-199511000-00022. PMID: 8595200.
Amboss-Artikel Hypophyse https://next.amboss.com/de/article/jK0_TS?q=pomc#CPcqSc0 (Zuletzt abgerufen: 31.07.2024)
Amboss-Artikel Haut und Hautanhangsgebilde: https://next.amboss.com/de/article/so0tWS#IloyMDJiNmU5YTQwZGRjZTYwM2Q5YzYyZmI0NjgwNTIyNiI= (Zuletzt abgerufen: 31.07.2024)
Amboss-Artikel Hirnstamm
https://next.amboss.com/de/article/yo0deS?q=periaqu%C3%A4duktales%20grau#Ze49a70f5b344df1c31083fd9c99d1348 (Zuletzt abgerufen: 31.07.2024)
Robinson KC, Kemény LV, Fell GL, Hermann AL, Allouche J, Ding W, Yekkirala A, Hsiao JJ, Su MY, Theodosakis N, Kozak G, Takeuchi Y, Shen S, Berenyi A, Mao J, Woolf CJ, Fisher DE. Reduced MC4R signaling alters nociceptive thresholds associated with red hair. Sci Adv. 2021 Apr 2;7(14):eabd1310. doi: 10.1126/sciadv.abd1310. PMID: 33811065; PMCID: PMC11057701.
Meuser T, Ameis A, Lehmann KA: Haben Patienten mit roten Haaren ein höheres Risiko für
Komplikationen in Anästhesie und Schmerztherapie? Eine kritische Auswertung der Literatur.
Anästh Intensivmed 2019;60:57–64. DOI: 10.19224/ai2019.057
Blutungsanamnese:
Kumar VV, Kumar NV, Isaacson G. Superstition and post-tonsillectomy hemorrhage. Laryngoscope. 2004 Nov;114(11):2031-3. doi: 10.1097/01.mlg.0000147942.82626.1c. PMID: 15510037.
Liem EB, Hollensead SC, Joiner TV, Sessler DI. Women with red hair report a slightly increased rate of bruising but have normal coagulation tests. Anesth Analg. 2006 Jan;102(1):313-8. doi: 10.1213/01.ANE.0000180769.51576.CD. PMID: 16368849; PMCID: PMC1351323.
Angst und Aufregung:
Binkley CJ, Beacham A, Neace W, Gregg RG, Liem EB, Sessler DI. Genetic variations associated with red hair color and fear of dental pain, anxiety regarding dental care and avoidance of dental care. J Am Dent Assoc. 2009 Jul;140(7):896-905. doi: 10.14219/jada.archive.2009.0283. PMID: 19571053; PMCID: PMC2740987.
Dawson DV. Variants in the melanocortin-1 receptor (MC1R) gene appear to be associated with increased dental care-related anxiety, increased fear of dental pain, and greater likelihood of dental care avoidance. J Evid Based Dent Pract. 2010 Sep;10(3):169-71. doi: 10.1016/j.jebdp.2010.05.007. PMID: 20797666.
Randall CL, McNeil DW, Shaffer JR, Crout RJ, Weyant RJ, Marazita ML. Fear of Pain Mediates the Association between MC1R Genotype and Dental Fear. J Dent Res. 2016 Sep;95(10):1132-7. doi: 10.1177/0022034516661151. PMID: 27555332; PMCID: PMC5004243.
Mavrogiorgou, P., Zogas, H., Zogas, G. et al. Perioperative Ängste und die Angst vor dem Tod. Anaesthesiologie 72, 266–272 (2023). https://doi.org/10.1007/s00101-023-01267-3
Midazolam
Chua MV, Tsueda K, Doufas AG. Midazolam causes less sedation in volunteers with red hair. Can J Anaesth. 2004 Jan;51(1):25-30. doi: 10.1007/BF03018542. PMID: 14709456.
Narkose- und Überwachungsverfahren
Meretsky CR, Plitt VE, Friday BL, Schiuma AT, Ajebli M. A Comparative Analysis of the Efficacy of Local Anesthetics and Systemic Anesthetics in the Red-Headed Versus Non-Red-Headed Patient Population: A Comprehensive Review. Cureus. 2024 Jun 6;16(6):e61797. doi: 10.7759/cureus.61797. PMID: 38975446; PMCID: PMC11227258.
Augustinsson A, Franze E, Almqvist M, Warrén Stomberg M, Sjöberg C, Jildenstål P. Red-Haired People’s Altered Responsiveness to Pain, Analgesics, and Hypnotics: Myth or Fact?-A Narrative Review. J Pers Med. 2024 May 29;14(6):583. doi: 10.3390/jpm14060583. PMID: 38929804; PMCID: PMC11204720.
Meuser T, Ameis A, Lehmann KA: Haben Patienten mit roten Haaren ein höheres Risiko für
Komplikationen in Anästhesie und Schmerztherapie? Eine kritische Auswertung der Literatur.
Anästh Intensivmed 2019;60:57–64. DOI: 10.19224/ai2019.057
Lidocain:
Liem EB, Joiner TV, Tsueda K, Sessler DI. Increased sensitivity to thermal pain and reduced subcutaneous lidocaine efficacy in redheads. Anesthesiology. 2005 Mar;102(3):509-14. doi: 10.1097/00000542-200503000-00006. PMID: 15731586; PMCID: PMC1692342.
Algesimetrie
Freye, E., Grabitz, K., & Latasch, L. (2003). Bestimmung der analgetischen Tiefe während der Anästhesie: Rationale zum Einsatz somatosensorisch-evozierter Potentiale – eine Übersicht. A&I Online. Abgerufen von https://www.ai-online.info/images/ai-ausgabe/2000/02-2000/AI208.PDF, abgerufen am 09.01.2025
Gracely et al. A multiple random staircase method of psychophysical pain assessment, Pain. 1988 Jan;32(1):55-63
Bromm B, Meier W. The intracutaneous stimulus: a new pain model for algesimetric studies., Methods Find Exp Clin Pharmacol 1984 Jul;6(7):405-10
Gruenewald M, Ilies C. Monitoring the nociception-anti-nociception balance. Best Pract Res Clin Anaesthesiol. 2013 Jun;27(2):235-47. doi: 10.1016/j.bpa.2013.06.007. PMID: 24012235.
Link zur Firma Medtronic: https://www.medtronic.com/covidien/de-de/products/nociception-analgesia-management/nol-pain-technology.html#
Martini C.H. et al (2015), Ability of the Nociception Level (NOL), a multiparameter composite of autonomic signals, to detect noxious stimuli during anesthesia. Anesthesiology Sept. 2015; 123:524-534
Meijer, F. et al (2019). Nociception-guided versus Standard Care during Anesthesia: A Randomized Controlled Trial. Anesthesiology, 130(5), 745-755. doi:10.1097/ALN.000000000000263
Komplikationen von Immuncheckpoint-Inhibitoren
Chan KK, Bass AR. Autoimmune complications of immunotherapy: pathophysiology and management. BMJ. 2020 Apr 6;369:m736. doi: 10.1136/bmj.m736. PMID: 32253223.
Yan T, Yu L, Zhang J, Chen Y, Fu Y, Tang J, Liao D. Achilles‘ Heel of currently approved immune checkpoint inhibitors: immune related adverse events. Front Immunol. 2024 Feb 12;15:1292122. doi: 10.3389/fimmu.2024.1292122. PMID: 38410506; PMCID: PMC10895024.
Salem JE, Manouchehri A, Moey M, Lebrun-Vignes B, Bastarache L, Pariente A, Gobert A, Spano JP, Balko JM, Bonaca MP, Roden DM, Johnson DB, Moslehi JJ. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 2018 Dec;19(12):1579-1589. doi: 10.1016/S1470-2045(18)30608-9. Epub 2018 Nov 12. PMID: 30442497; PMCID: PMC6287923.
Kroschinsky F, Stölzel F, von Bonin S, Beutel G, Kochanek M, Kiehl M, Schellongowski P; Intensive Care in Hematological and Oncological Patients (iCHOP) Collaborative Group. New drugs, new toxicities: severe side effects of modern targeted and immunotherapy of cancer and their management. Crit Care. 2017 Apr 14;21(1):89. doi: 10.1186/s13054-017-1678-1. PMID: 28407743; PMCID: PMC5391608.
Gutierrez C, McEvoy C, Munshi L, Stephens RS, Detsky ME, Nates JL, Pastores SM. Critical Care Management of Toxicities Associated With Targeted Agents and Immunotherapies for Cancer. Crit Care Med. 2020 Jan;48(1):10-21. doi: 10.1097/CCM.0000000000004087. PMID: 31725440; PMCID: PMC7505092.
Schneider BJ, Naidoo J, Santomasso BD, Lacchetti C, Adkins S, Anadkat M, Atkins MB, Brassil KJ, Caterino JM, Chau I, Davies MJ, Ernstoff MS, Fecher L, Ghosh M, Jaiyesimi I, Mammen JS, Naing A, Nastoupil LJ, Phillips T, Porter LD, Reichner CA, Seigel C, Song JM, Spira A, Suarez-Almazor M, Swami U, Thompson JA, Vikas P, Wang Y, Weber JS, Funchain P, Bollin K. Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: ASCO Guideline Update. J Clin Oncol. 2021 Dec 20;39(36):4073-4126. doi: 10.1200/JCO.21.01440. Epub 2021 Nov 1. Erratum in: J Clin Oncol. 2022 Jan 20;40(3):315. doi: 10.1200/JCO.21.02786. PMID: 34724392.
Dine J, Gordon R, Shames Y, Kasler MK, Barton-Burke M. Immune Checkpoint Inhibitors: An Innovation in Immunotherapy for the Treatment and Management of Patients with Cancer. Asia Pac J Oncol Nurs. 2017 Apr-Jun;4(2):127-135. doi: 10.4103/apjon.apjon_4_17. PMID: 28503645; PMCID: PMC5412150.
Podcast: Play in new window | Download

Wie immer eine inhaltlich sehr interessante Folge.
Nur diese obligatorische „Orwellsche 5-Minuten-Politik“ war wieder mal etwas… undurchsichtig:
1. „Fuck Nazis“ – klar, keine Diskussion. Auch wenn ich mir nicht sicher bin, wie viele davon regelmäßig auf medizinischen Fachkongressen anzutreffen sind – aber geschenkt.
2. Die AfD – ja, keine sympathische Truppe. Sie sind nationalistisch, ja. Also sozusagen das Gegenteil von Globalisten. Beides gibt’s, beides hat Vor- und Nachteile. Ich bin völlig einverstanden, dass wir in einer globalisierten Welt leben und dass Globalisten vielleicht besser auf die heutigen Herausforderungen reagieren können als Nationalisten. Trotzdem: Nationalisten (also Leute, die Probleme auf Ebene des Nationalstaats lösen wollen) mit Nazis (Eugenik, Holocaust, Weltkrieg) gleichzusetzen, ist einfach historisch und sachlich falsch.
Dann diese Argumentation à la „Ich sage das, um den Leuten die Angst zu nehmen“ – ernsthaft? Die offiziellen Positionen der Regierung und fast aller großen Medien mutig zu wiederholen ist jetzt also der neue Widerstand? Wie viele AfD-Anhänger waren wohl bei Grünen- oder Linken-Parteitagen “zu Gast”? Und wie oft ist es andersherum bei AfD- oder neuerlich sogar CDU-Veranstaltungen passiert? Wer sollte da eigentlich wovor Angst haben?
Manche Dinge bleiben eben rätselhaft.
Und rein aus Interesse: Sind die zwei Hosts eigentlich genau in der Zeit der Ampel-Koalition in die Schweiz und nach England gezogen, weil dort die Grenzen offener sind und die Regierungen „linker“? Fragen über Fragen.
Lieber Lukas,
Danke für deinen Kommentar. Den Orwell-Vergleich sehen wir auf jeden Fall als Lob, denn ähnlich wie Orwell zu seiner Zeit beobachten auch wir die heutigen rechten Tendenzen mit großer Sorge. Deiner Einschätzung der AFD kann ich leider nicht zustimmen, weil ich sehr dort sehr deutliche Tendenzen, die über Nationalismus hinaus- und sehr deutlich in eine nationalsozialistische Richtung gehen. Daher halten wir es für angebracht diese Sorge auch in unserem Podcast, auf Kongressen etc. zu äußern und hier eine klare Kante zu zeigen. Es ist dir natürlich frei gestellt das anders zu sehen.
Und um das Rätsel um meinen Wohnort zu lösen: ich bin unter anderem in die Schweiz und zeitweise nach England gezogen, um andere Länder und Gesundheitssysteme kennenzulernen und meinen Horizont zu erweitern, sehr globalistische Beweggründe also 😉
Liebe Grüße,
Paula und das Team der Pin-up Docs
Moin,
habt ihr zum Lieblingsfehler Hintergrundinfo zur Geschichte? Ich habe die Problematik in unserer Abteilung angesprochen und jetzt „darf“ ich dazu eine Info für alle verfassen und das möchte ich mit ein wenig Leben füllen. Vielen Dank!
Hallo Cord,
entschuldige bitte.. Dein Kommentar ist uns komplett durchgerutscht.. Leider haben wir keinerlei weitere Hintergrund-Infos dazu bekommen.. Also können wir Dir noch nicht mal helfen, aber ggf. kannst du an die Firma BRAUN direkt herantreten?
Lieben Gruß und nochmals grosses SORRY!
Dana und der Rest des Teams